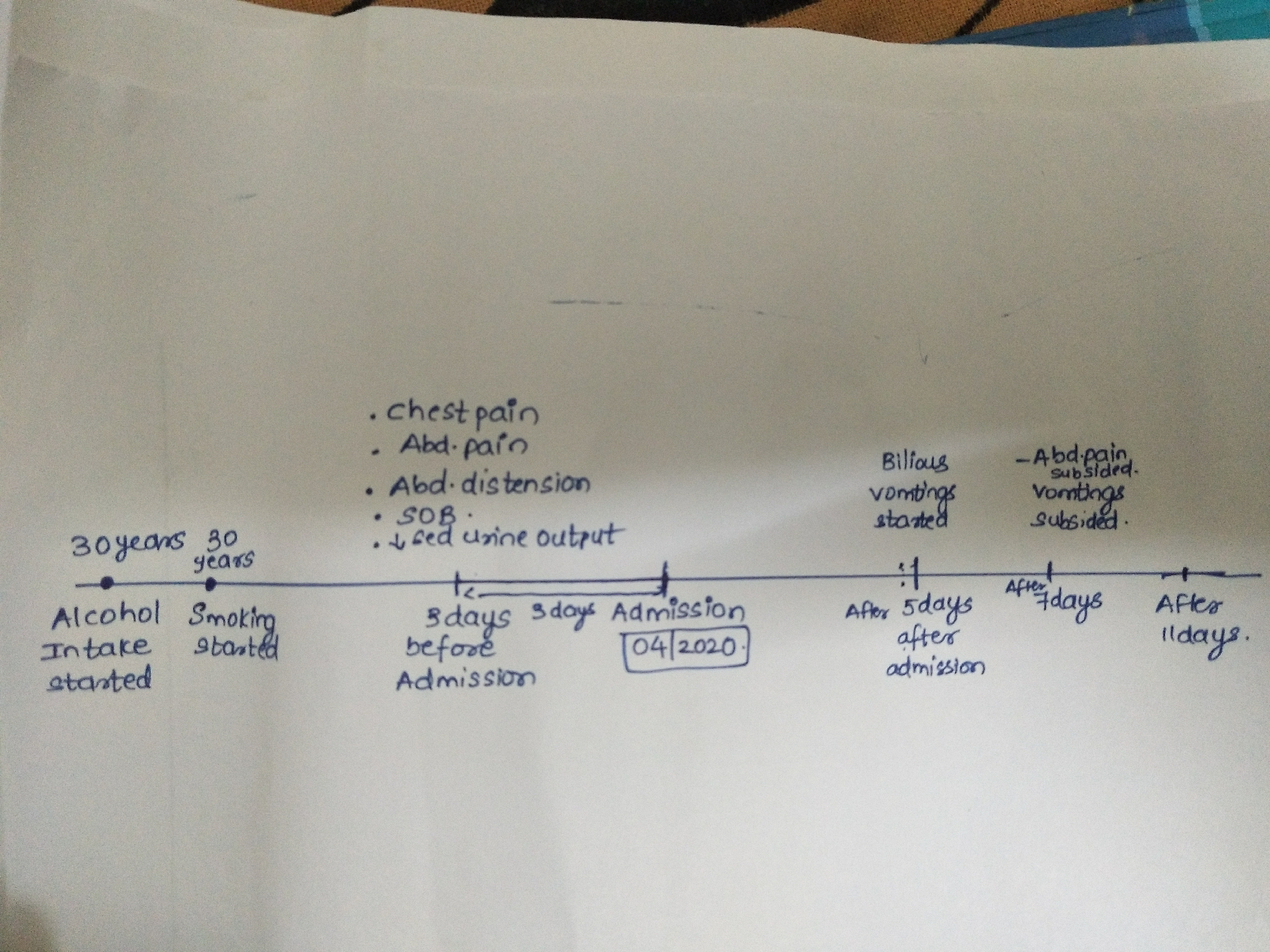
A 30 year old lady with a known case of seizures since 4years.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case presentation:
A 30 year old lady who is labourer by occupation came with chief complaints of multiple seizure episodes since 4 years.
Patient was apparently asymptomatic 4years back and then she had an episode of seizure for which she was hospitalised and diagnosed as NCC and is treated with ALBENDAZOLE-400mg LEVIPIL-500mg and OMNACORTIL.
She is having on and off seizures from then(yearly once) inspite of regular medication.(LEVIPIL 500mg)
Recently LEVIPIL was replaced with PHENYTOIN 100mg 6months back and she had increased frequency and severity of seizures from then.
On 1/10/2020 she had three episodes of GTC seizures continuously from 9pm each episode lasted for 10minutes patient regained consciousness in between the episodes, increase of tone in both upper and lower limbs, deviation of mouth to left was present, uprolling of eyes was present, no involuntary passage of urine and stools. No tongue biting and frothing.she was taken to local hospital and treated and the seizure was subsided
On 5/10/2020 she had three episodes of gtc seizures, each episode lasting for 10 minutes with increased tone of both upper and lower limbs, deviation of mouth to left, frothing and tongue biting was present. Up rolling of eyes was present, consciousness was regained in between the seizures, no involuntary passage of urine and stools seizure free interval was 10minutes between each episode. She was taken to the local hospital and treated and the seizures subsided.
No h/o headache, vomiting, blurring of vision, diplopia
No h/o fever, neck pain, tingling and numbness. No h/o urine and faecal incontinence.
Past history :
Not k/c/o DM, HTN, Asthma, CAD, TB
No known drug allergies and no relevant family history.
Diet is mixed with normal appetite and adequate sleep, with regular bowel and bladder movements.
General examination :
Patient is conscious, coherent and cooperative who is well built and well nourished.
No signs of pallor, icteris, cyanosis, clubbing, lypmphadenopathy and edema.
Vitals
Patient is afebrile
BP 110/70mm Hg recorded in right arm in sitting position
PR 84bpm regular
RR 24cpm
SYSTEMIC EXAMINATION
CVS- s1 s2 heard no murmur
RESPIRATORY SYSTEM -bilateral air entry present , + normal vesicular breath sounds. no added sounds.Traches central in position
PER ABDOMEN-
Scaphoid in shape,no tenderness and no palpable mass present.Hernial orifices are free.Liver and spleen are not palpable.Bowel sounds are present.
CNS:
Higher motor funtions normal
patient is conscious and oriented to place/time/person.
All cranial nerves- intact
MOTOR SYSTEM
Left. Right
Bulk: inspection Normal normal palpation Normal Normal
Measurements U/L Equal on both sides
L/L Equal on both sides
Tone:
UL Normal Increased
LL Normal Normal
Power :
UL 5/5 5/5
LL 4+/5 4+/5
Reflexes: absent
SENSORY SYSTEM
RIGHT. LEFT
SPINOTHALAMIC
crude touch. N. N
pain. N. N
temperature. N. N
post:
fine touch. N. N
vibration. N. N
position sensor. N. N
cortical
2 point discrimination N. N
tactile localisation. N. N
CEREBELLAR SIGNS - normal
No meningeal signs
INVESTIGATIONS:
MRI scan done in 2017
MRI scan done in 2017MRI scan done in 2018MRI scan done on 5/10/2020MRI scan done on 5/10/2020
On 10/10/2020
LFT
RFT
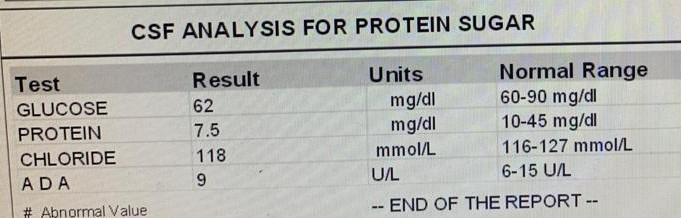
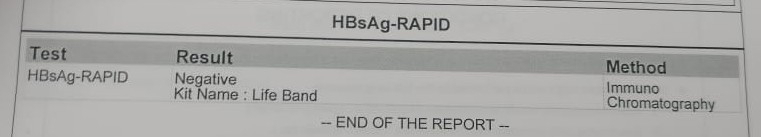
Csf analysis.
Serology
DIAGNOSIS:
GTCS secondary to ? NCC or Tuberculoma.
TREATMENT:
1) Tab levipil 500mg/PO/BD
2) Tab pan 40mg OD
3)Inj Optineuron 1amp in 100 ml NS IV/BD
4) Tab Dicorate ER 300mg PO/ BD
5) Tab Albendazole 400mg BD
6) Tab wysolone 30mg OD 1week followed by 20mg OD 1week followed by 10mg OD 1week followed by 5mg OD 1week
7) GRBS charting 8th hourly
8)Temperature charting
9)plenty of oral fluids
10)BP charting 2hourly
11)monitor vitals