A 54 year old male with cough,abdominal tightness,pedal edema and diarrhea.
Here is the case I have seen-
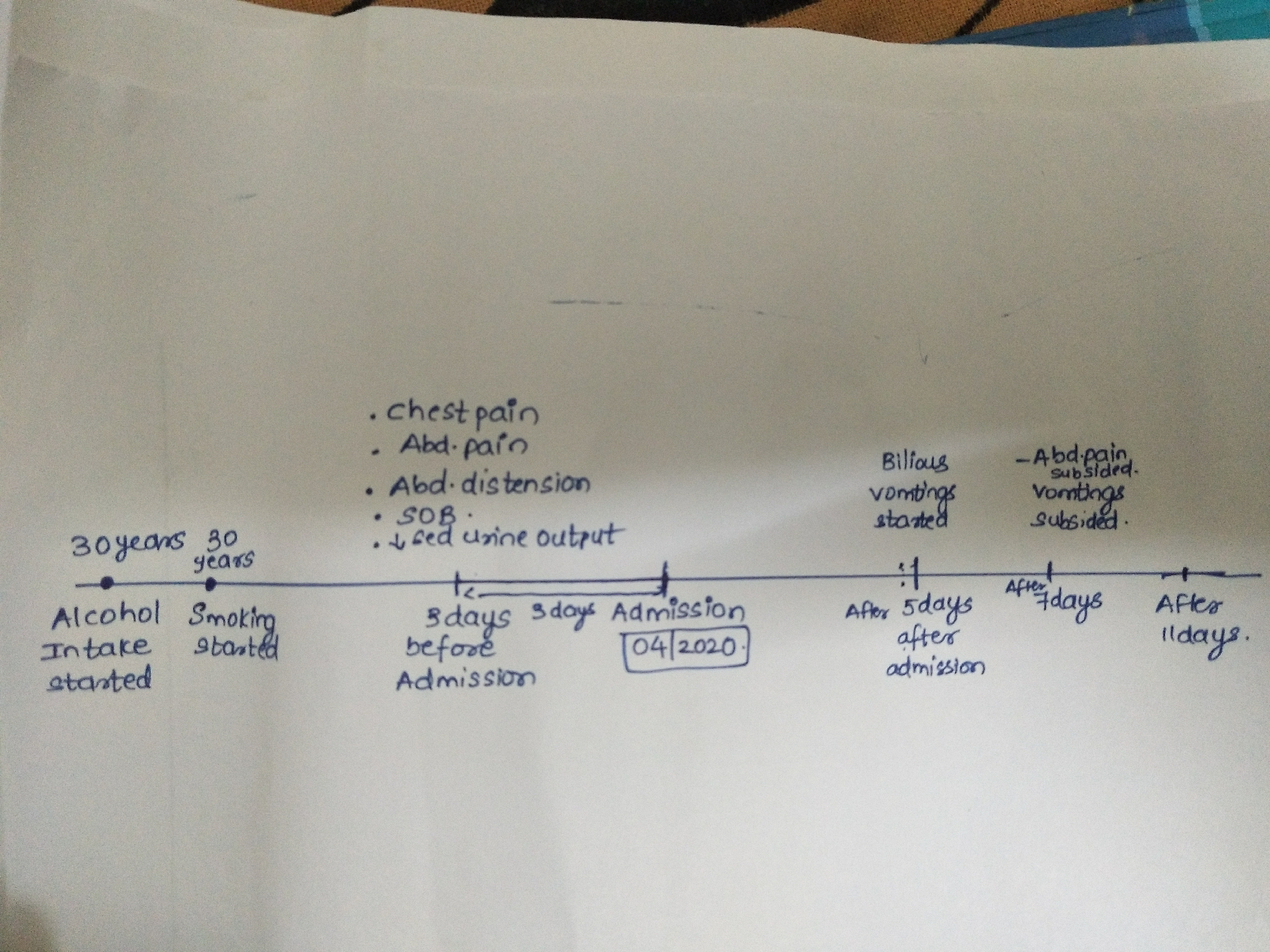
A 54 year old male ,weaver by occupation,residing at nalgonda was apparently alright 8 years back. Due to financial loss and family problems,he started drinking exessively from then.On december 9th 2019,he was admitted in hospital for seizures (diagnosed as alcohol withdrawal seizures, as he stopped drinking for 10 days)- GTCS for 2 minutes associated with uprolling of eye balls,frothing from mouth,post ictal confusion,No involuntary passage of stools,urination ,no loss of consciousness.Again 2 episodes of seizures occurred during the stay in hospital where loss of consciousness present.There,in the hospital he was also diagnosed as chronic pancreatitis, cholelithiasis,alcohol liver disease and was advised for complete abstinence from alcohol.
In January 2020,he started drinking again.whenever he drinks,he takes less amount of food.During lockdown period,he stopped drinking as wine shops were closed. again started drinking when the shops opened.
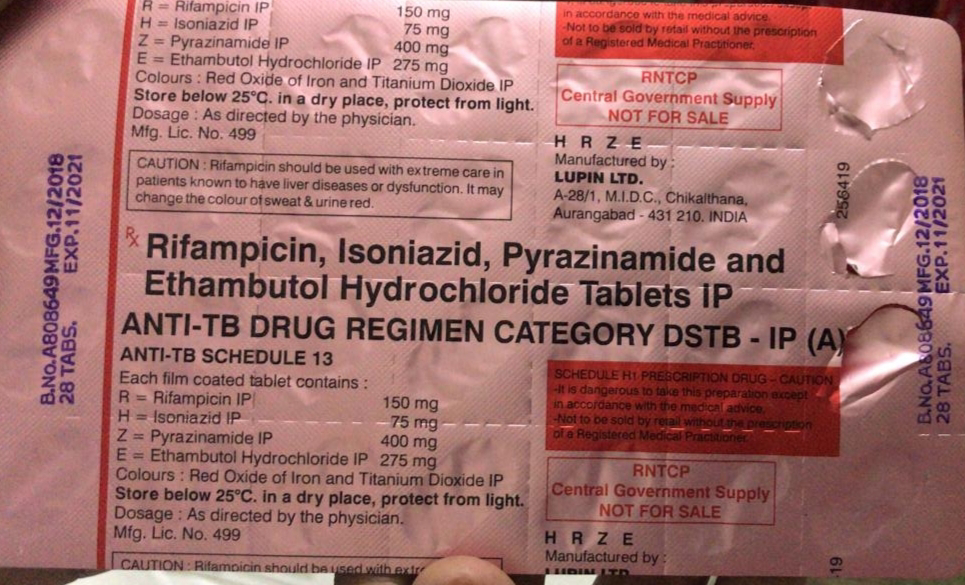
In july 2020, he started having fever - low grade which relieves on taking medication (on and off) more during nights,not associated with chills, rigors and sweating.It is associated with dry cough- more at night,insidious in onset,progressive in nature,more on lying down position.he was also complaining of Generalised weakness from july, most of the time, confined to bed.On july 18th,he had dog bite to his right knee(had vaccination 4 doses).For these symptoms,he got COVID Ag test done in july,turned out to be negative.In september,he started having abdominal tightness(after taking spicy foods ),pedal edema - pitting type (on and off) shortness of breath, all symptoms from 1 month for which he was referred to govt hospital where he was diagnosed as sputum positive TB and started ATT - 3 tablets at once after break fast(now,it is his 4th day using them).H/o loose stools from 20 days watery in consistency,non foul smelling, no mucus,2 to 3 episodes per day.not associated with pain abdomen , vomitings.
PAST HISTORY
K/c/o diabetes since 8 years and is on metformin 500mg and glimiperide 2 mg
K/c/o HTN since 3yrs and is on irregular medication(atenolol 50mg and amlodipine 5mg).
Pulmonary kochs - from 3 days, he is on ATT
PERSONAL HISTORY:
Married, weaver by occupation
Diet - mixed
Loss of appetite,disturbed sleep due to cough.
Bowel and bladder movements- normal
He is alcoholic from 35 years, drinks daily.
General physical examination:
Patient is conscious,coherent,cooperative
Looks emaciated
Weight -40 kgs , abdominal girth -77cms
Icterus present.pedal edema present
No pallor,cyanosis ,clubbing,koilonycia and lympadenopathy.
Vitals:
Temp 98.6F
PR 108
RR 20 cycles/ min
BP 130/90 mm of hg
Spo2 98% at room air
Grbs 72 mg/dl.
SYSTEMIC EXAMINATION.
CVS : S1 S2 heard, no murmurs.
RS : B/l air entry present, NVBS heardMotor system- intact
Sensory system - intact
Cranial nerve examination- normal
INVESTIGATIONS :
USG REPORT
Day2:
Day 3
Day 4Day 5:Day6:CT report on 24/9/20
CECT Abdomen report on 24/9/2020Diagnosis - pulmonary koch's with chronic liver disease with chronic pancreatitis with type 2 DM with hyponatremia secondary to SIADH (pulmonary koch's) with gross ascites(transudative).
TREATMENT:
INJ. PIPTAZ 2.25 gm/IV/TID
INJ. VIT-K 10 mg IV OD for 7 days
TAB.METROGYL 400mg BD
TAB.RIDOTIL 100mg BD
TAB.RIFAGUT 550mg BD
TAB.SPOROLAC-DS TID
INJ.Human Actrapid Insulin s/c 8am - 2pm - 8pm
INJ.PAN 40 mg IV/OD
INJ.OPTINEURON 1 amp in 100 ml NS IV/BD
ATT to be with held
Protein powder 3 to 4 scoops in 1 glass of milk or water QID
Stop all OHA s
Grbs charting 6th hrly
Strict I/0 charting
High protein diet 4eggs daily
ORS sachets in 1 litre of water
Bp charting hourly
Temp BP PR monitoring 4th hourly
IVF - 1 DNS , 1NS @50ml/hr
Nebulisation with salbutamol and mucomist 12th hourly
INJ.THIAMINE 100 mg in 100 ml NS IV TID.